Ultimate Guide to Severe Anal Fissure Healing-2024
Introduction:
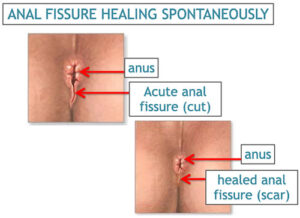
Ultimate Guide to Severe Anal Fissure Healing-2024. An anal fissure is a small tear or crack in the lining of the anus, which can cause pain, bleeding, and discomfort during bowel movements. Although it is a common condition, the symptoms can be distressing and affect one’s quality of life. Understanding the causes, symptoms, and treatment options for anal fissures can help individuals manage and alleviate this condition effectively.
Understanding Anal Fissures
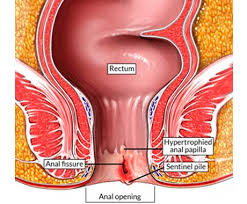
An anal fissure occurs when there is a tear in the skin of the anal canal. This tear can be caused by various factors, such as trauma from passing large or hard stools, chronic diarrhea, or inflammatory bowel diseases. The tear exposes the underlying muscles, leading to pain and discomfort, particularly during and after bowel movements.
Causes of Anal Fissures
Several factors can contribute to the development of anal fissures:
Constipation and Hard Stools
Straining during bowel movements and passing large or hard stools is the most common cause of anal fissures. This increased pressure can cause the delicate tissue in the anal canal to tear, leading to a fissure.
Chronic Diarrhea
Frequent bowel movements and diarrhea can irritate and damage the anal lining. The constant passage of loose stools can wear down the protective lining, making it more susceptible to tearing.
Inflammatory Bowel Diseases
Conditions such as Crohn’s disease and ulcerative colitis cause chronic inflammation of the digestive tract, including the anus. This inflammation can make the tissue more fragile and prone to fissures.
Trauma
Trauma to the anal area, such as from anal intercourse or the insertion of foreign objects, can cause tears in the lining of the anus. Even aggressive wiping after bowel movements can lead to fissures.
Childbirth
The strain and pressure during childbirth can result in anal fissures. The perineal area, including the anus, is subjected to significant stress during delivery, increasing the risk of tears.
Decreased Blood Flow
Reduced blood flow to the anorectal area, often seen in older adults, can impair the healing of small tears. Conditions that affect circulation, such as peripheral artery disease, can also contribute to this issue.
Muscle Spasms
Increased tension and spasms of the anal sphincter muscle can prevent healing and exacerbate fissures. When the muscle tightens, it reduces blood flow to the area, hindering the natural healing process.

Symptoms of Anal Fissures
Ultimate Guide to Severe Anal Fissure Healing-2024 can cause a range of symptoms, including:
Pain During Bowel Movements
Sharp, severe pain during and after bowel movements is the most common symptom. The pain is often described as feeling like passing shards of glass. This pain can last from minutes to hours after a bowel movement, making the experience particularly distressing.
Bleeding
Bright red blood on toilet paper or in the toilet bowl after a bowel movement is a common symptom. This bleeding is usually minimal but can be alarming. The blood is often fresh and not mixed with the stool, distinguishing it from other types of rectal bleeding.
Itching and Irritation
Persistent itching and irritation around the anus can occur due to the fissure. The broken skin and inflammation can lead to an itchy sensation that can be quite uncomfortable.
Visible Tear
A small tear or crack in the skin around the anus may be visible. This can often be seen during a physical examination by a healthcare provider. The fissure is typically located at the posterior midline of the anus but can occur at other locations as well.
Discomfort
A persistent feeling of discomfort or soreness in the anal area is common. This discomfort can be constant or fluctuate throughout the day, often worsening during bowel movements.
Spasm
Involuntary tightening or spasming of the anal sphincter muscle, which can worsen pain and hinder healing. These spasms can be a natural response to pain but can perpetuate the cycle of discomfort and difficulty in healing.
Diagnosis
Diagnosing an anal fissure typically involves a physical examination and medical history review:
Visual Inspection
A doctor can usually diagnose an anal fissure by visually inspecting the area around the anus. The fissure is typically easy to spot and can be seen as a small tear or ulceration.
Digital Rectal Examination (DRE)
In some cases, a digital rectal examination may be performed to check for abnormalities or underlying conditions. This involves the doctor inserting a lubricated, gloved finger into the rectum to feel for any irregularities. However, due to the pain associated with fissures, this examination is often avoided if the diagnosis can be made visually.
Anoscopy
An anoscope, a small tubular instrument, may be used to examine the inside of the anal canal for further evaluation. This tool allows the doctor to get a closer look at the fissure and assess its severity.
Treatment Options
Treatment for anal fissures aims to relieve symptoms, promote healing, and prevent recurrence. Options include:
Lifestyle Changes
Dietary Adjustments
Increasing fiber intake through fruits, vegetables, and whole grains can help soften stools and reduce straining. A high-fiber diet can promote regular bowel movements and make stools easier to pass, reducing the risk of further trauma to the anal area.
Hydration
Drinking plenty of water helps keep stools soft and easier to pass. Adequate hydration is essential for maintaining overall digestive health and preventing constipation.
Avoiding Straining
Not delaying bowel movements and avoiding excessive straining can prevent further trauma to the anal area. Using the bathroom as soon as the urge arises and not spending too much time on the toilet can help mitigate the risk of fissures.
Home Remedies
Warm Sitz Baths
Sitting in warm water for 10-15 minutes several times a day can relax the anal muscles and promote healing. The warmth helps to soothe the pain and can also improve blood flow to the area, aiding in the healing process.
Topical Treatments
Over-the-counter creams and ointments containing hydrocortisone or lidocaine can reduce inflammation and pain. These products can provide temporary relief from symptoms and help manage the discomfort associated with fissures.
Cold Compresses
Applying ice packs to the affected area can help reduce swelling and numb the area. Cold therapy can be particularly useful in managing acute pain and inflammation.
Medical Treatments
Topical Nitroglycerin
This prescription ointment helps relax the anal sphincter muscle and improve blood flow, promoting healing. Nitroglycerin works by dilating blood vessels, which can enhance circulation to the fissure site and facilitate the healing process.
Calcium Channel Blockers
Topical medications like diltiazem or nifedipine can relax the anal sphincter and facilitate healing. These medications are often used when nitroglycerin is not effective or causes side effects.
Botox Injections
Botulinum toxin injections can temporarily paralyze the anal sphincter muscle, reducing spasms and allowing the fissure to heal. This treatment is particularly useful for chronic fissures that have not responded to other therapies.
Surgery
In cases where conservative treatments fail, surgical options like lateral internal sphincterotomy can be considered. This procedure involves making a small incision in the anal sphincter muscle to reduce tension and promote healing. It is highly effective but comes with risks, such as incontinence.
Detailed Analysis of Medical Treatments
Topical Nitroglycerin
Topical nitroglycerin is one of the first-line treatments for anal fissures. It works by relaxing the internal anal sphincter muscle, which reduces pressure in the anal canal and improves blood flow to the fissure, promoting healing. Common side effects include headaches and dizziness, which are related to the vasodilatory effects of the medication. Patients typically apply the ointment twice daily for several weeks. While effective, adherence to the treatment regimen is crucial for optimal results.

Calcium Channel Blockers
Calcium channel blockers, such as diltiazem and nifedipine, are used topically to treat anal fissures. These medications also relax the internal anal sphincter muscle and improve blood flow to the area. They are often prescribed when nitroglycerin is not effective or causes intolerable side effects. Patients generally apply the medication two to three times daily. Studies have shown that calcium channel blockers can be as effective as nitroglycerin with fewer side effects.
Botox Injections
Botulinum toxin, commonly known as Botox, is injected into the internal anal sphincter muscle to temporarily paralyze it. This reduces spasms and pressure, allowing the fissure to heal. The effects of Botox last for several months, providing a window for the fissure to heal completely. Botox injections are typically performed in an outpatient setting and require minimal recovery time. Patients may experience mild discomfort at the injection site, but serious side effects are rare.
Lateral Internal Sphincterotomy
Lateral internal sphincterotomy is a surgical procedure that involves making a small incision in the internal anal sphincter muscle to reduce tension and promote healing of the fissure. This procedure is highly effective, with success rates exceeding 90%. However, it carries risks, including incontinence and infection. The procedure is usually reserved for chronic fissures that do not respond to medical treatments. Recovery time varies, but most patients return to normal activities within a few weeks.
Complications of Untreated Anal Fissures
If left untreated, anal fissures can lead to complications, including:
Chronic Fissure
Persistent fissures that do not heal within 6-8 weeks may become chronic and require more aggressive treatment. Chronic fissures are more difficult to treat and may require surgical intervention.
Infection
The tear can become infected, leading to abscess formation and requiring medical intervention. Signs of infection include increased pain, redness, swelling, and pus discharge from the fissure.
Anal Fistula
In some cases, a fissure can develop into an anal fistula, an abnormal connection between the anal canal and the skin around the anus, which may require surgical treatment. Fistulas can cause persistent drainage and recurrent infections.
Preventive Measures
Preventing anal fissures involves addressing the underlying causes and adopting healthy habits:
High-Fiber Diet
Consuming a diet rich in fiber can prevent constipation and reduce the risk of fissures. Foods such as fruits, vegetables, whole grains, and legumes are excellent sources of dietary fiber. Fiber supplements, such as psyllium husk, can also be beneficial for individuals who struggle to meet their fiber needs through diet alone.
Hydration
Drinking adequate water helps maintain soft stools and ease bowel movements. Aim for at least 8 glasses of water a day, or more if you are physically active or live in a hot climate.
Regular Exercise
Physical activity promotes healthy bowel function and prevents constipation. Activities such as walking, jogging, and swimming can stimulate intestinal motility and improve overall digestive health.
Avoid Straining
Using proper bathroom habits, such as not delaying bowel movements and avoiding excessive straining, can prevent fissures. Respond to the urge to defecate promptly and avoid prolonged sitting on the toilet, which can increase pressure on the anal area.
Good Hygiene
Maintaining good anal hygiene can prevent irritation and reduce the risk of infection. Gently cleaning the anal area with mild soap and water after bowel movements and avoiding harsh or scented products can help maintain healthy skin integrity.
Psychological Impact
Living with anal fissures can have a significant psychological impact. Chronic pain, discomfort, and the fear of bowel movements can lead to anxiety and stress. It is important to address these psychological aspects as part of a comprehensive treatment plan. Counseling or therapy can be beneficial for managing stress and anxiety related to the condition.
Support and Resources
Support from healthcare professionals, including gastroenterologists and colorectal surgeons, is essential for managing Ultimate Guide to Severe Anal Fissure Healing-2024. Additionally, support groups and online forums can provide valuable information and emotional support from others experiencing similar issues. Connecting with others who have experienced similar challenges can provide comfort and practical advice.
When to See a Doctor
It is essential to seek medical attention if:
Symptoms Persist
If symptoms do not improve with home treatment or over-the-counter medications, it is important to consult a healthcare provider. Persistent symptoms may indicate a chronic fissure or an underlying condition that requires medical evaluation.
Severe Pain
Intense pain or swelling requires medical evaluation. Severe pain can be a sign of complications such as an abscess or infection.
Excessive Bleeding
Persistent or heavy bleeding warrants a doctor’s visit. While minor bleeding is common with fissures, significant or prolonged bleeding may indicate a more serious issue.
Changes in Bowel Habits
Significant changes in bowel habits or stool appearance should be investigated. Changes such as persistent diarrhea, constipation, or the presence of blood or mucus in the stool may indicate an underlying gastrointestinal condition.
Conclusion
Anal fissures are a common condition that can cause significant pain and discomfort. Understanding the causes, symptoms, and treatment options is crucial for effective management and relief. Lifestyle changes, dietary adjustments, home remedies, and medical treatments can all play a role in treating and managing this condition. Preventive measures, such as maintaining a healthy diet and avoiding straining, can help reduce the risk of fissures. Additionally, addressing the psychological impact and seeking support from healthcare professionals and support groups can improve overall well-being. If you are experiencing symptoms of an anal fissure, it is important to consult with a healthcare provider to develop an individualized treatment plan tailored to your specific needs.