Table of Contents
ToggleComprehensive Guide to Internal Hemorrhoid Treatment
Overview:
Internal hemorrhoids, while often a source of discomfort, are a common medical condition that can be effectively managed with a variety of treatment options. This guide provides a detailed overview of internal hemorrhoids, their causes, symptoms, diagnosis, and treatment strategies, ranging from conservative home remedies to advanced medical procedures.
Understanding Internal Hemorrhoids:
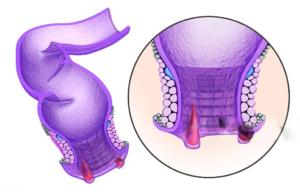
Internal hemorrhoids are swollen blood vessels that develop inside the rectum, typically unnoticed until they cause symptoms. They are categorized into four grades based on their severity:
- Grade 1: These are small, internal swellings that usually do not prolapse and are often painless.
- Grade 2: These hemorrhoids may prolapse during bowel movements but retract back into the anus on their own.
- Grade 3: These prolapse out of the anus during bowel movements and require manual repositioning.
- Grade 4: These are permanently prolapsed and cannot be pushed back in. They may become strangulated and cause severe pain.
Causes and Risk Factors
The development of internal hemorrhoids can be attributed to increased pressure in the lower rectum. This pressure can result from various factors:
- Straining during bowel movements: Often due to constipation or diarrhea.
- Pregnancy: The increased pressure on the pelvic veins during pregnancy.
- Obesity: Excess weight can put pressure on the abdominal and pelvic areas.
- Prolonged sitting or standing: Can increase the pressure on the veins in the anus.
- Low-fiber diet: Leads to hard stools and straining during bowel movements.
- Aging: The tissues supporting the veins in the rectum and anus can weaken with age.
- Chronic diarrhea or constipation: Frequent bowel movements or hard stools can strain the rectal veins.
- Heavy lifting: Regularly lifting heavy objects can increase abdominal pressure.
Symptoms of Internal Hemorrhoids
Symptoms vary depending on the severity of the hemorrhoids and may include:
- Painless rectal bleeding: Bright red blood on toilet paper, in the toilet bowl, or in the stool.
- Prolapse: Hemorrhoids that protrude outside the anus, which may cause discomfort and require manual repositioning.
- Itching and irritation: Caused by mucus discharge and inflammation of the surrounding skin.
- Discomfort during bowel movements: A feeling of incomplete evacuation or a sensation of pressure.
- Pain: Severe pain is uncommon unless the hemorrhoid becomes thrombosed (clotted) or strangulated.
Diagnosis of Internal Hemorrhoids
Accurate diagnosis is crucial for effective treatment and typically involves:
- Medical History and Symptom Review: Discussion of symptoms and potential risk factors.
- Physical Examination: Includes a digital rectal examination (DRE) where the doctor uses a gloved finger to feel for abnormalities inside the rectum.
- Anoscopy: A small, lighted tube is inserted into the anus to visualize internal hemorrhoids directly.
- Sigmoidoscopy: Allows the doctor to examine the lower part of the colon and rectum using a flexible tube with a light and camera.
- Colonoscopy: A more extensive examination that can visualize the entire colon, often recommended if there are signs of other gastrointestinal issues or if symptoms persist despite treatment.
Conservative Treatments
For mild to moderate internal hemorrhoids, conservative treatments can often provide significant relief:
- Dietary Changes:
- Increase Fiber Intake: Consuming more fruits, vegetables, whole grains, and fiber supplements helps soften stools and reduce straining.
- Hydration: Drinking plenty of fluids (especially water) helps prevent constipation and keeps stools soft.
- Over-the-Counter Medications:
- Topical Creams and Ointments: Products containing hydrocortisone or witch hazel can reduce inflammation and itching.
- Suppositories: Help deliver medication directly to the affected area to relieve symptoms.
- Sitz Baths: Soaking the anal area in warm water for 10-15 minutes, several times a day, can help soothe irritation and reduce inflammation.
- Stool Softeners: Medications that help soften stools, making them easier to pass and reducing the need for straining.
- Lifestyle Modifications:
- Avoid Prolonged Sitting: Taking breaks to stand and move around can reduce pressure on the rectal veins.
- Exercise Regularly: Physical activity helps stimulate bowel function and reduces constipation.
- Proper Bathroom Habits: Avoid delaying bowel movements, and do not sit on the toilet for extended periods.
Medical Procedures for Internal Hemorrhoids
When conservative treatments are insufficient, medical procedures may be necessary to treat internal hemorrhoids effectively:
- Rubber Band Ligation (RBL):
- Procedure: A rubber band is placed around the base of the hemorrhoid to cut off its blood supply, causing it to shrink and fall off.
- Indication: Commonly used for grade 2 and some grade 3 hemorrhoids.
- Recovery: Minimal recovery time is needed, and normal activities can usually be resumed immediately.
- Sclerotherapy:
- Procedure: A chemical solution is injected into the hemorrhoid, causing it to shrink.
- Indication: Suitable for treating small to medium-sized hemorrhoids.
- Recovery: Quick recovery with minimal discomfort.
- Infrared Coagulation (IRC):
- Procedure: Uses infrared light to create scar tissue, cutting off the blood supply to the hemorrhoid.
- Indication: Effective for treating smaller hemorrhoids.
- Recovery: Generally involves little to no downtime.
- Electrocoagulation:
- Procedure: An electric current is applied to the hemorrhoid, causing it to harden and shrink.
- Indication: Suitable for small to medium-sized hemorrhoids.
- Recovery: Quick recovery, with some minor discomfort possible.
Advanced Surgical Procedures
For severe or recurrent hemorrhoids, advanced surgical procedures may be required:
- Hemorrhoidectomy:
- Procedure: Surgical removal of the hemorrhoid tissue.
- Indication: Best for large, prolapsed, or thrombosed hemorrhoids and when other treatments have failed.
- Recovery: Requires a longer recovery period, often several weeks, with potential for significant pain and discomfort.
- Hemorrhoidal Artery Ligation (HAL):
- Procedure: Uses Doppler ultrasound to locate and tie off the arteries supplying the hemorrhoid.
- Indication: Effective for treating complex or recurrent hemorrhoids.
- Recovery: Typically involves a shorter recovery period than a traditional hemorrhoidectomy.
- Stapled Hemorrhoidopexy:
- Procedure: Uses a stapling device to remove excess hemorrhoidal tissue and reposition the remaining tissue.
- Indication: Often used for prolapsed hemorrhoids.
- Recovery: Generally involves less pain and a shorter recovery time compared to traditional surgery.
- Transanal Hemorrhoidal Dearterialization (THD):
- Procedure: Similar to HAL, it involves ligating the hemorrhoidal arteries but focuses on reducing blood flow to the hemorrhoids without excision.
- Indication: Suitable for complex or recurrent hemorrhoids.
- Recovery: Shorter recovery time with less post-operative pain.
Post-Procedure Care and Recovery

Recovery and aftercare are crucial for successful treatment outcomes and preventing recurrence:
- Pain Management:
- Medications: Prescription or over-the-counter pain relievers as recommended by the healthcare provider.
- Sitz Baths: Regular sitz baths can provide relief and aid healing.
- Wound Care:
- Dressings: Applying and changing dressings as needed to keep the area clean and promote healing.
- Hygiene: Keeping the anal area clean and dry is essential to prevent infection.
- Diet and Hydration:
- Fiber and Fluids: Continue with a high-fiber diet and adequate fluid intake to avoid constipation.
- Stool Softeners: Use as directed to prevent straining during bowel movements.
- Activity Restrictions:
- Rest: Avoid strenuous activities and heavy lifting during the initial recovery period.
- Gradual Return to Normal Activities: Follow the healthcare provider’s advice on resuming normal activities and exercise.
Complications and Risks
While treatments for internal hemorrhoids are generally safe, they can carry potential risks and complications:
- Bleeding: Some bleeding is expected after procedures, but significant or prolonged bleeding should be reported to a healthcare provider.
- Infection: Rare but possible, especially after surgical procedures.
- Recurrence: Hemorrhoids may return, particularly if lifestyle changes are not maintained.
- Anal Fissure: The development of a tear in the anal lining can occur after some treatments.
- Fecal Incontinence: Rarely, procedures involving the anal sphincter muscles can lead to issues with bowel control.
Preventing Recurrence
To prevent the recurrence of internal hemorrhoids and maintain overall colorectal health, consider these lifestyle modifications:
- Dietary Fiber:
- High-Fiber Foods: Include plenty of fruits, vegetables, legumes, and whole grains in your diet.
- Fiber Supplements: Consider using supplements like psyllium husk if dietary intake is insufficient.
- Hydration:
- Adequate Fluid Intake: Drink plenty of water throughout the day to help soften stools.
- Regular Exercise:
- Physical Activity: Engage in regular exercise to promote healthy bowel function and reduce the risk of constipation.
- Healthy Bathroom Habits:
- Avoid Straining: Do not strain during bowel movements; use stool softeners if necessary.
- Respond Promptly to Bowel Urges: Do not delay going to the bathroom when you feel the urge.
- Limit Toilet Time: Avoid sitting on the toilet for extended periods.
- Weight Management:
- Healthy Weight: Maintaining a healthy weight can reduce pressure on the rectal veins.
- Posture and Movement:
- Avoid Prolonged Sitting: Stand and move around regularly, especially if you have a sedentary job.
When to Seek Medical Advice
Seek medical attention if you experience any of the following:
- Persistent rectal bleeding or a change in bowel habits.
- Severe pain or discomfort not relieved by over-the-counter treatments.
- Signs of infection such as fever, increased pain, redness, or swelling.
- Prolapsed hemorrhoids that do not respond to manual repositioning.
- Symptoms persist or worsen despite treatment.
Conclusion
Internal hemorrhoids are a common condition that can significantly impact quality of life, but they can be effectively managed with a range of treatments. From dietary changes and over-the-counter remedies to advanced medical procedures, understanding the available options and making informed choices is crucial for effective management and relief. Preventative measures, lifestyle modifications, and seeking timely medical advice can help manage symptoms and reduce the likelihood of recurrence. If you suspect you have internal hemorrhoids or are experiencing symptoms, consult with a healthcare provider to determine the best treatment approach for your individual needs.
By addressing symptoms promptly and adopting healthy habits, individuals can manage internal hemorrhoids effectively and enjoy improved colorectal health.
I love the examples you provided.
Thanks. And many more upcoming. good day