Finally External Hemorrhoid Recurrence Grade 2:
Introduction:
Hemorrhoids are a widespread issue that impacts a significant portion of the population, often causing considerable discomfort and distress. External hemorrhoids, particularly at Grade 2 severity, can be especially bothersome due to their location and the symptoms they manifest. This detailed article explores Grade 2 external hemorrhoids, covering their causes, symptoms, diagnosis, treatment options, and preventive measures in-depth.
What Are Hemorrhoids?
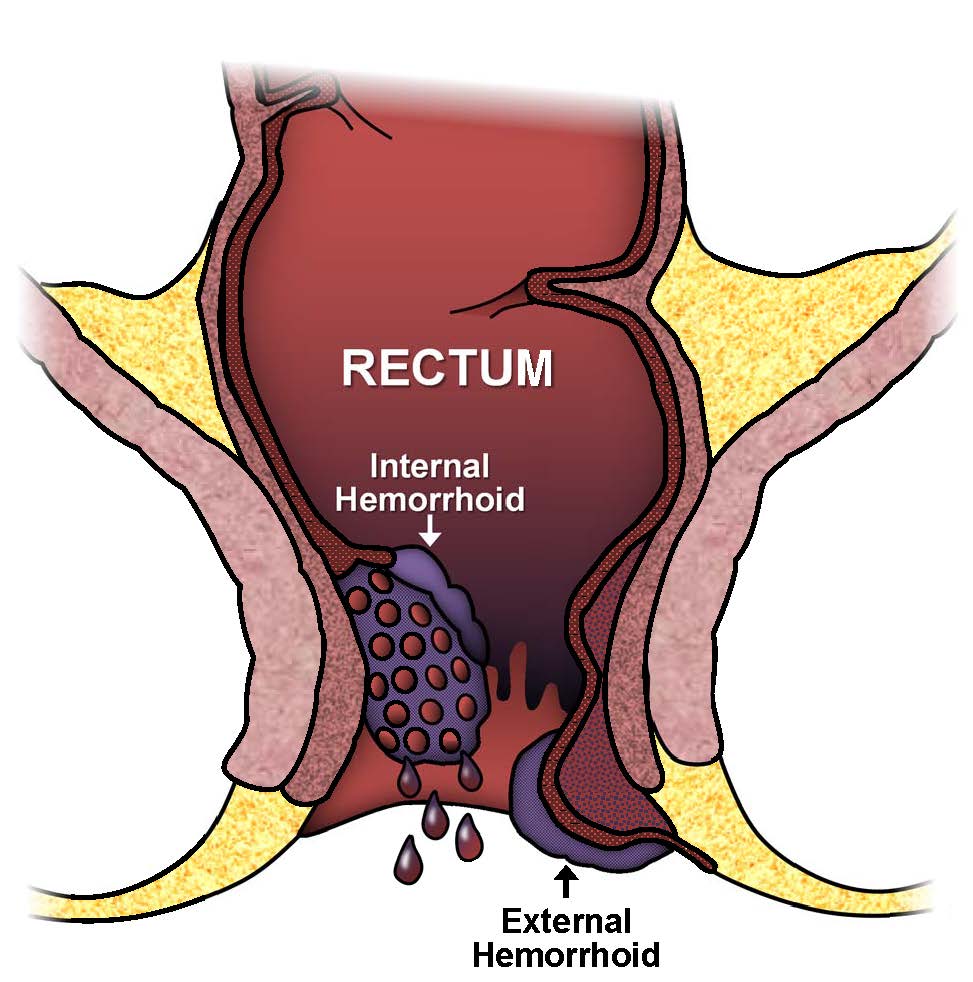
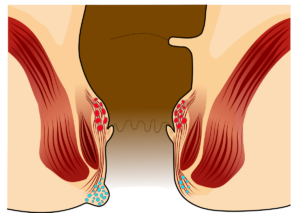
Hemorrhoids are enlarged, swollen blood vessels in the lower rectum and anus. They are a common condition, with varying degrees of severity and impact. Hemorrhoids can be internal or external:
- Internal Hemorrhoids: These occur within the rectum and are generally not visible or painful unless they prolapse or cause bleeding.
- External Hemorrhoids: These form under the skin around the anus, often resulting in significant discomfort and pain due to their location and exposure to friction and irritation.
External Hemorrhoid Recurrence Grade 2: Classification:
External hemorrhoids are classified based on their severity and degree of prolapse:
- Grade 1: Hemorrhoids are present with swelling and inflammation around the anus but no prolapse.
- Grade 2: Hemorrhoids prolapse during bowel movements or other activities but retract spontaneously.
- Grade 3: Hemorrhoids prolapse during bowel movements and require manual reduction to return them inside.
- Grade 4: Hemorrhoids are prolapsed and remain outside the anus permanently, often requiring surgical intervention.
Grade 2 hemorrhoids represent a moderate level of severity and are the focus of this article.
Understanding Grade 2 External Hemorrhoids
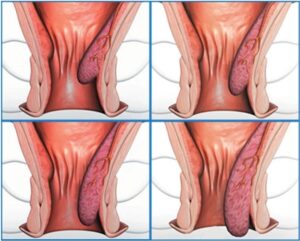
Grade 2 external hemorrhoids are characterized by swollen veins that extend outside the anus during bowel movements or other activities that increase intra-abdominal pressure. Unlike more severe grades, these hemorrhoids spontaneously retract back into the anal canal after the precipitating activity ceases.
Causes of Finally External Hemorrhoid Recurrence Grade 2:
Several factors contribute to the development of Grade 2 external hemorrhoids. Understanding these can help in managing and preventing their occurrence:
- Chronic Straining: Straining during bowel movements due to constipation or hard stools increases pressure in the anal veins, leading to their swelling and prolapse.
- Constipation: Difficulty in passing stools causes prolonged straining, which can lead to the development and worsening of hemorrhoids.
- Diarrhea: Frequent loose stools can irritate and inflame the anal region, contributing to hemorrhoid formation.
- Prolonged Sitting: Sitting for long periods, especially on the toilet, increases pressure on the anal veins, facilitating hemorrhoid development.
- Pregnancy: Hormonal changes and the physical pressure from the growing uterus during pregnancy can cause or exacerbate hemorrhoids.
- Obesity: Excess body weight places additional pressure on the pelvic and rectal veins, increasing the risk of hemorrhoids.
- Low-Fiber Diet: A diet lacking in fiber can lead to harder stools and more straining, both of which are risk factors for hemorrhoids.
- Aging: As people age, the tissues supporting the veins in the rectum and anus can weaken, making hemorrhoids more likely.
Symptoms of Grade 2 External Hemorrhoids
Grade 2 external hemorrhoids can present with a variety of symptoms, ranging from mild discomfort to significant pain:
- Prolapse: The hallmark of Grade 2 hemorrhoids is prolapse, where the swollen veins extend outside the anus during bowel movements or activities that increase intra-abdominal pressure, but retract on their own.
- Pain and Discomfort: The protruding hemorrhoids can cause substantial pain and discomfort, particularly during and after bowel movements.
- Itching and Irritation: The prolapsed hemorrhoid can lead to persistent itching and irritation around the anus due to mucus secretion and skin contact.
- Swelling: Noticeable swelling and lumps around the anal area are common with external hemorrhoids.
- Bleeding: Bright red blood may be seen on toilet paper or in the stool, stemming from the delicate and swollen veins.
- Difficulty Cleaning: Prolapsed hemorrhoids can complicate hygiene, making it difficult to clean the anal area effectively.
Diagnosing Grade 2 External Hemorrhoids
Diagnosing Grade 2 external hemorrhoids typically involves a thorough physical examination and a review of the patient’s medical history. Healthcare professionals may employ several methods to confirm the diagnosis:
- Visual Inspection: A visual examination of the anal area can identify any visible swelling or prolapse indicative of external hemorrhoids.
- Digital Rectal Exam: Inserting a gloved, lubricated finger into the rectum allows the doctor to feel for abnormalities within the anal canal.
- Anoscopy: Using an anoscope, a small, lighted tube, the doctor can view the inside of the anal canal and rectum to assess the presence and severity of hemorrhoids.
- Proctoscopy: This is a more extensive examination compared to anoscopy, allowing for a detailed view of the rectum to evaluate any internal hemorrhoids or other issues.
These diagnostic tools help in distinguishing hemorrhoids from other conditions with similar symptoms, such as anal fissures, fistulas, or colorectal cancer.
Treatment Options for Grade 2 External Hemorrhoids
Treatment for Grade 2 external hemorrhoids aims to relieve symptoms, reduce inflammation, and prevent further complications. Options range from conservative treatments to more invasive procedures, depending on the severity of symptoms and the patient’s overall health.
Conservative Treatments:
Initial management of Grade 2 external hemorrhoids often involves conservative treatments, which include lifestyle changes and over-the-counter (OTC) remedies:
- Dietary Changes: Increasing fiber intake through foods like fruits, vegetables, and whole grains helps soften stools and reduce straining. Fiber supplements, such as psyllium or methylcellulose, can also be beneficial.
- Hydration: Drinking plenty of water throughout the day prevents dehydration, which can lead to constipation and hard stools.
- Topical Treatments: OTC creams, ointments, and suppositories containing ingredients like hydrocortisone or witch hazel can provide relief from itching, pain, and inflammation.
- Warm Sitz Baths: Soaking the anal area in warm water for 10-15 minutes several times a day can reduce pain and swelling. Adding Epsom salts can enhance the soothing effect.
- Pain Relievers: Non-prescription pain relievers such as acetaminophen, ibuprofen, or aspirin can help manage discomfort and reduce inflammation.
- Avoiding Straining: Patients are advised to avoid straining during bowel movements and to respond promptly to the urge to defecate to minimize pressure on the anal veins.
Minimally Invasive Procedures:
When conservative treatments are insufficient, minimally invasive procedures may be considered. These procedures are typically performed in an outpatient setting and involve minimal discomfort and recovery time:
- Rubber Band Ligation: A small rubber band is placed around the base of the hemorrhoid to cut off its blood supply, causing it to wither and fall off within a few days. This procedure is effective for treating internal hemorrhoids and can sometimes be adapted for external ones.
- Sclerotherapy: A chemical solution is injected into the hemorrhoid, causing it to shrink and eventually disappear. This method is often used for internal hemorrhoids but can be applied to external ones under certain conditions.
- Infrared Coagulation (IRC): This technique uses infrared light to coagulate the blood vessels in the hemorrhoid, reducing its size. It is typically used for internal hemorrhoids but can also be adapted for external hemorrhoids.
- Cryotherapy: Freezing the hemorrhoid with liquid nitrogen causes it to shrink and die. This method can be effective but may require multiple sessions and has a higher recurrence rate compared to other treatments.
These procedures are generally effective and offer a balance between efficacy and invasiveness, making them suitable for many patients with Grade 2 hemorrhoids.
Surgical Interventions:
For persistent or severe cases where other treatments have failed, surgical intervention may be necessary. Surgical options for Grade 2 external hemorrhoids include:
- Hemorrhoidectomy: This involves the surgical removal of hemorrhoids. While highly effective, it is usually reserved for severe cases due to the pain and longer recovery time associated with the procedure.
- Hemorrhoidopexy (Stapled Hemorrhoidectomy): Also known as stapled hemorrhoidectomy, this procedure involves stapling the prolapsed hemorrhoid back into place inside the rectum. It is less painful than a traditional hemorrhoidectomy and has a shorter recovery period.
- Laser Surgery: Laser energy is used to vaporize or excise the hemorrhoidal tissue. This method is associated with less postoperative pain and a quicker recovery compared to traditional surgery.
Surgical options are typically considered when other treatments have not provided sufficient relief or when hemorrhoids significantly impact the patient’s quality of life.
Preventing Grade 2 External Hemorrhoids:
Preventive measures are crucial in managing and reducing the recurrence of hemorrhoids. These strategies focus on minimizing the risk factors associated with hemorrhoid formation:
- High-Fiber Diet: Consuming a diet rich in fiber helps maintain regular bowel movements and reduces the need to strain. Foods such as whole grains, fruits, vegetables, and legumes are excellent sources of fiber.
- Staying Hydrated: Drinking adequate water helps prevent constipation and maintain soft stools. It is recommended to drink at least 8-10 glasses of water per day.
- Regular Exercise: Engaging in physical activity promotes regular bowel movements and reduces pressure on the rectal veins. Activities like walking, swimming, and yoga are beneficial.
- Avoiding Prolonged Sitting: Limiting the time spent sitting, especially on the toilet, reduces pressure on the anal veins. Taking breaks to stand or walk can help alleviate this pressure.
- Responding Promptly to Bowel Urges: Delaying bowel movements can lead to constipation and increased straining. It is important to heed the body’s natural urges to defecate.
- Maintaining a Healthy Weight: Managing body weight reduces the pressure on the pelvic and rectal areas, lowering the risk of developing hemorrhoids.
- Proper Toilet Habits: Avoiding excessive straining and using gentle cleaning methods can help prevent hemorrhoid irritation and inflammation. Using moistened toilet paper or wipes can be gentler on the anal area.
Complications of Grade 2 External Hemorrhoids:
While Grade 2 external hemorrhoids are typically manageable with appropriate treatment, complications can arise if they are left untreated or improperly managed:
- Thrombosis: Blood clots can form within the hemorrhoid, leading to severe pain, swelling, and inflammation. Thrombosed hemorrhoids may require surgical intervention to relieve the pain and remove the clot.
- Infection: Prolapsed hemorrhoids can become infected, especially if hygiene is compromised. This can lead to abscess formation and require antibiotic treatment or surgical drainage.
- Chronic Prolapse: Over time, untreated Grade 2 hemorrhoids can progress to more severe grades, leading to persistent prolapse and the need for surgical correction.
- Anemia: Chronic bleeding from hemorrhoids can result in anemia, characterized by fatigue, weakness, and pallor. This is more common with internal hemorrhoids but can occur with external ones as well.
When to See a Doctor:
While many cases of Grade 2 external hemorrhoids can be managed with home treatments and lifestyle changes, it is important to seek medical attention if:
- Symptoms persist or worsen despite treatment.
- There is significant bleeding from the rectum.
- The hemorrhoids are causing severe pain or discomfort.
- There are signs of infection, such as fever, increased redness, or swelling around the anus.
A healthcare provider can offer appropriate diagnosis and treatment options to manage symptoms and prevent complications.
Conclusion:
Grade 2 external hemorrhoids represent a moderate stage of hemorrhoid disease, characterized by prolapse during bowel movements and spontaneous retraction. They can cause significant discomfort and impact daily life, but a range of treatment options is available to manage symptoms and prevent progression. Understanding the causes, symptoms, and treatment options for Grade 2 external hemorrhoids is essential for effective management and improved quality of life.
By adopting preventive measures, such as maintaining a high-fiber diet, staying hydrated, and avoiding prolonged sitting, individuals can reduce their risk of developing hemorrhoids. Early intervention and appropriate treatment can alleviate symptoms and prevent the progression to more severe stages, ensuring better health and comfort.