External Hemorrhoid Grade 3: Comprehensive Overview of Causes, Symptoms, and Treatments
Introduction External Hemorrhoid Grade 3: Comprehensive Overview:
External Hemorrhoid Grade 3: Comprehensive Overview. Hemorrhoids, commonly known as piles, are swollen veins in the lower rectum and anus. They can be internal or external. This article focuses on external hemorrhoids, specifically Grade 3, which represents a more advanced and problematic stage of the condition. Understanding the causes, symptoms, and available treatments for Grade 3 external hemorrhoids is crucial for effective management and relief.
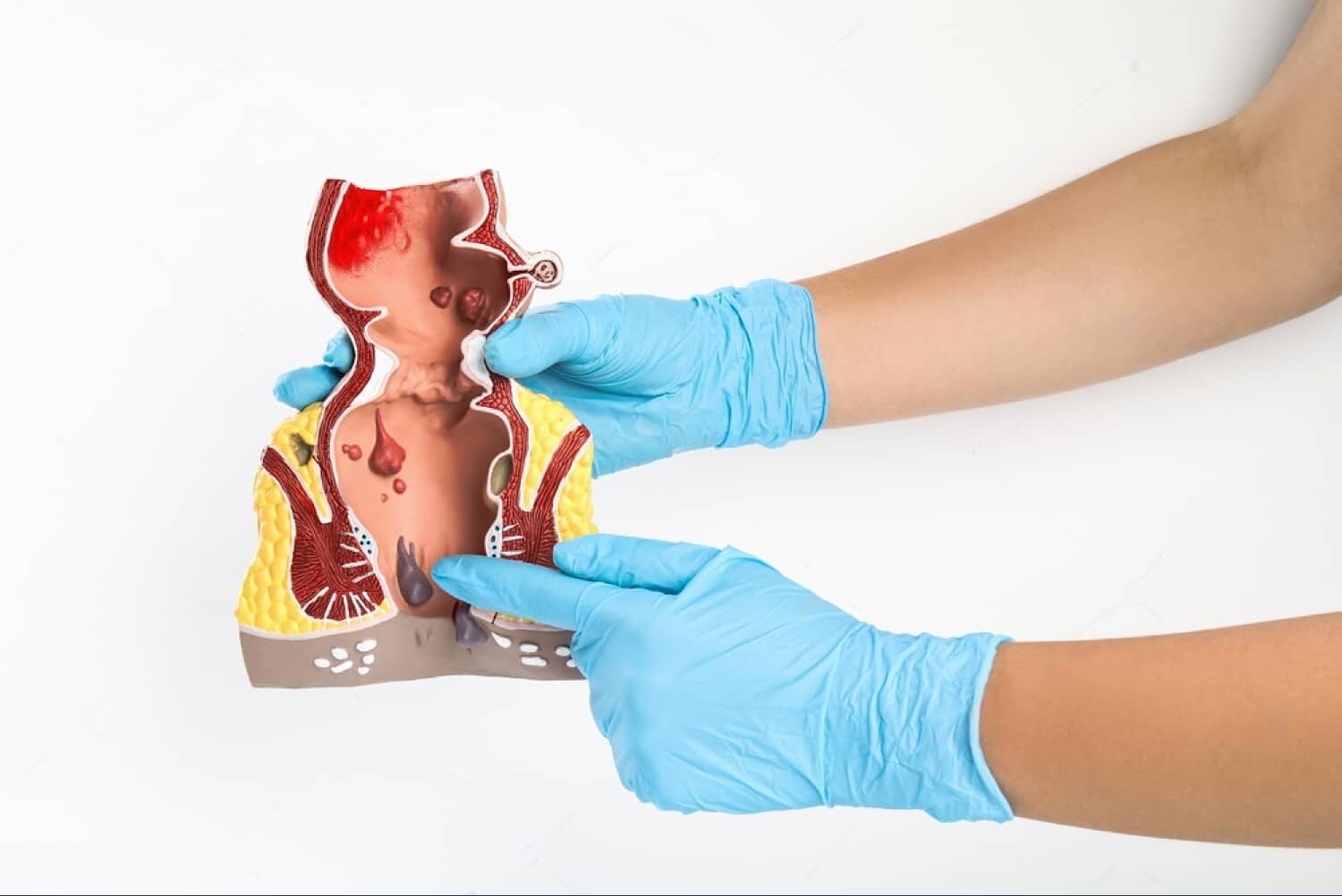
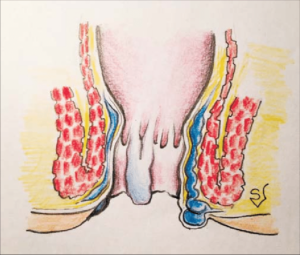
What are External Hemorrhoids?
External hemorrhoids are found under the skin surrounding the anus. They can cause significant discomfort and pain, particularly when thrombosed (clotted) or inflamed. External hemorrhoids are generally more painful than internal hemorrhoids, which occur inside the rectum.
Classification of Hemorrhoids
Hemorrhoids are classified into four grades based on their severity:
- Grade 1: Hemorrhoids are slightly enlarged but do not prolapse (they stay inside the anus).
- Grade 2: Hemorrhoids prolapse during bowel movements but retract spontaneously.
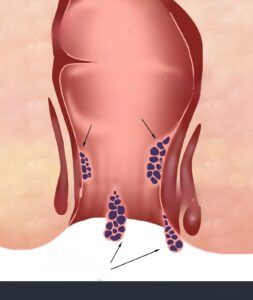
- Grade 3: Hemorrhoids prolapse during bowel movements and need to be manually pushed back into the anus.
- Grade 4: Hemorrhoids are permanently prolapsed and cannot be pushed back in.
Understanding External Hemorrhoid Grade 3
External Hemorrhoid Grade 3 refers to hemorrhoids that protrude from the anus during bowel movements or physical exertion and do not retract on their own. Instead, they must be manually pushed back inside. These hemorrhoids are more severe than Grade 2 and require more intensive treatment to manage symptoms and prevent complications.
Causes of External Hemorrhoid Grade 3: Comprehensive Overview:
Several factors contribute to the development of external hemorrhoids, including:
- Straining during Bowel Movements: Excessive straining increases pressure on the veins in the rectum and anus, leading to swelling and prolapse.
- Chronic Constipation or Diarrhea: Both conditions can exacerbate hemorrhoids. Constipation causes straining, while diarrhea can lead to irritation and inflammation.
- Prolonged Sitting: Sitting for long periods, especially on the toilet, can increase pressure on the rectal veins.
- Obesity: Excess body weight puts additional pressure on the pelvic veins, contributing to hemorrhoid formation.
- Pregnancy: The increased pressure on the pelvic area during pregnancy can cause hemorrhoids. Hormonal changes also play a role.
- Low-Fiber Diet: A diet low in fiber can lead to constipation and straining, which are significant risk factors for hemorrhoids.
- Aging: As people age, the tissues supporting the veins in the rectum and anus can weaken, leading to hemorrhoids.
Symptoms of External Hemorrhoid Grade 3: Comprehensive Overview:
The symptoms of Grade 3 external hemorrhoids can vary but typically include:
- Pain and Discomfort: Pain is a common symptom, especially during bowel movements. The pain can range from mild to severe.
- Itching and Irritation: The area around the anus can become itchy and irritated, leading to further discomfort.
- Swelling: Swelling around the anus is common and can be felt as a lump.
- Bleeding: Bright red blood on toilet paper or in the toilet bowl after a bowel movement is a common sign of hemorrhoids.
- Prolapse: Hemorrhoids that protrude during bowel movements and must be manually pushed back inside.
Diagnosis
Diagnosing external hemorrhoid Grade 3 typically involves:
- Physical Examination: A doctor will examine the area around the anus to check for swelling and prolapse.
- Digital Rectal Examination (DRE): The doctor may insert a lubricated, gloved finger into the rectum to feel for abnormalities.
- Anoscopy: A small, tubular instrument called an anoscope may be used to view the inside of the anal canal.
Treatment Options
Treatment for external hemorrhoid Grade 3 focuses on relieving symptoms and preventing further progression. Options include:
Lifestyle Changes:
- Diet: Increasing fiber intake through fruits, vegetables, and whole grains can help soften stools and reduce straining.
- Hydration: Drinking plenty of water can prevent constipation.
- Exercise: Regular physical activity can promote bowel regularity.
Over-the-Counter Medications:
- Topical Treatments: Creams, ointments, and suppositories containing hydrocortisone or witch hazel can reduce inflammation and pain.
- Pain Relievers: Non-prescription pain relievers like acetaminophen or ibuprofen can help alleviate discomfort.
Home Remedies:
- Warm Sitz Baths: Sitting in warm water for 10-15 minutes several times a day can reduce swelling and pain.
- Cold Compresses: Applying ice packs to the affected area can help reduce swelling and numb the area.
Medical Procedures:
- Rubber Band Ligation: A rubber band is placed around the base of the hemorrhoid to cut off blood supply, causing it to wither and fall off.
- Sclerotherapy: A chemical solution is injected into the hemorrhoid to shrink it.
- Infrared Coagulation: Infrared light is used to coagulate the blood vessels, causing the hemorrhoid to shrink.
- Hemorrhoidectomy: In severe cases, surgical removal of the hemorrhoid may be necessary.
Minimally Invasive Procedures:
- Stapled Hemorrhoidopexy: This procedure involves stapling the prolapsed hemorrhoid back into place, reducing blood flow to the hemorrhoid and causing it to shrink.
- Laser Therapy: Laser energy is used to cut off the blood supply to the hemorrhoid, causing it to shrink and fall off.
Preventive Measures
Preventing external hemorrhoids involves addressing the underlying causes. Effective measures include:
- Maintaining a Healthy Diet: A diet high in fiber and low in processed foods can prevent constipation and reduce straining.
- Staying Hydrated: Drinking sufficient water helps keep stools soft and easy to pass.
- Regular Exercise: Physical activity promotes healthy bowel function.
- Avoiding Prolonged Sitting: Taking breaks and avoiding sitting for long periods can reduce pressure on the rectal veins.
- Proper Bathroom Habits: Avoiding straining during bowel movements and not delaying the urge to defecate can prevent hemorrhoid formation.
Complications of Untreated Hemorrhoids
If left untreated, Grade 3 external hemorrhoids can lead to complications, including:
- Thrombosis: Blood clots can form within the hemorrhoid, causing severe pain and swelling.
- Anemia: Chronic blood loss from hemorrhoids can lead to anemia, characterized by fatigue and weakness.
- Strangulation: If the blood supply to a prolapsed hemorrhoid is cut off, it can become strangulated, leading to severe pain and infection.
When to See a Doctor
It is essential to seek medical attention if:
- Symptoms Persist: If symptoms do not improve with home treatment or over-the-counter medications.
- Severe Pain: Intense pain or swelling requires medical evaluation.
- Excessive Bleeding: Persistent or heavy bleeding warrants a doctor’s visit.
- Changes in Bowel Habits: Significant changes in bowel habits or stool appearance should be investigated.
Lifestyle and Dietary Adjustments
High-Fiber Diet: Incorporating high-fiber foods into your diet can significantly reduce the occurrence of constipation and straining. Examples include fruits like apples and pears, vegetables like broccoli and carrots, legumes such as beans and lentils, and whole grains like oats and brown rice.
Hydration: Adequate water intake is crucial. Aim for at least eight glasses of water a day to keep stools soft.
Regular Exercise: Engaging in regular physical activity, such as walking, swimming, or yoga, can improve bowel function and reduce the risk of hemorrhoids.
Avoid Prolonged Sitting: If your job requires long periods of sitting, take regular breaks to stand and move around. This helps alleviate pressure on the rectal veins.
Healthy Bathroom Habits: Do not delay bowel movements when you feel the urge. Straining during bowel movements can be minimized by using a footstool to elevate your feet, which changes the position of your rectum for easier passage of stools.
Medical Interventions
For Grade 3 external hemorrhoids that do not respond to conservative treatments, medical interventions may be necessary:
- Rubber Band Ligation: This procedure involves placing a rubber band around the base of the hemorrhoid to cut off its blood supply. The hemorrhoid will eventually wither and fall off. This is typically done in an outpatient setting and is effective for many patients.
- Sclerotherapy: In this procedure, a chemical solution is injected into the hemorrhoid, causing it to shrink. It is less invasive than surgery and can be performed in a doctor’s office.
- Infrared Coagulation: This technique uses infrared light to coagulate the blood vessels feeding the hemorrhoid, leading to its shrinkage. It is minimally invasive and can be done on an outpatient basis.
- Hemorrhoidectomy: For severe cases, surgical removal of the hemorrhoid may be required. This procedure is more invasive and typically reserved for hemorrhoids that do not respond to other treatments. Recovery can be more prolonged and painful, but it is often very effective.
- Stapled Hemorrhoidopexy: This procedure involves using a stapling device to reposition the prolapsed hemorrhoid and cut off its blood supply. It is less painful than traditional hemorrhoidectomy and has a shorter recovery time.
- Laser Therapy: Laser energy is used to cut off the blood supply to the hemorrhoid, causing it to shrink and fall off. It is a relatively new and less common treatment option.
Psychological Impact
Living with Grade 3 external hemorrhoids can have a significant psychological impact. Chronic pain, discomfort, and the fear of bleeding can lead to anxiety and stress. It is important to address these psychological aspects as part of a comprehensive treatment plan. Counseling or therapy can be beneficial for managing stress and anxiety related to the condition.
Support and Resources
Support from healthcare professionals, including gastroenterologists and colorectal surgeons, is essential for managing Grade 3 external hemorrhoids. Additionally, support groups and online forums can provide valuable information and emotional support from others experiencing similar issues.
Detailed Analysis of Medical Procedures
Rubber Band Ligation:
Rubber band ligation is one of the most common procedures for treating Grade 3 hemorrhoids. During this procedure, a rubber band is placed around the base of the hemorrhoid to cut off its blood supply. Within a few days, the hemorrhoid withers and falls off. This procedure is typically done in an outpatient setting and does not require anesthesia. Patients may experience some discomfort and bleeding after the procedure, but these symptoms are usually mild and resolve quickly.
Sclerotherapy:
Sclerotherapy involves injecting a chemical solution into the hemorrhoid, causing it to shrink. This procedure is less invasive than surgery and can be performed in a doctor’s office. The injection causes the walls of the hemorrhoid to collapse and stick together, reducing blood flow to the area. Sclerotherapy is generally well-tolerated, with minimal pain and quick recovery times. However, it may require multiple treatments to achieve the desired results.
Infrared Coagulation:
Infrared coagulation uses infrared light to coagulate the blood vessels feeding the hemorrhoid, leading to its shrinkage. This minimally invasive procedure is typically done on an outpatient basis. A special device is used to deliver infrared light to the hemorrhoid, causing the blood vessels to clot and the hemorrhoid to shrink. Patients usually experience little to no pain during the procedure and can return to normal activities shortly afterward.
Hemorrhoidectomy:
Hemorrhoidectomy is a surgical procedure used to remove severe hemorrhoids. This procedure is more invasive and typically reserved for hemorrhoids that do not respond to other treatments. Hemorrhoidectomy can be performed using various techniques, including traditional surgical removal, laser surgery, or stapled hemorrhoidopexy. Recovery from hemorrhoidectomy can be more prolonged and painful, but the procedure is often very effective in providing long-term relief.
Stapled Hemorrhoidopexy:
Stapled hemorrhoidopexy, also known as stapled hemorrhoidectomy, involves using a stapling device to reposition the prolapsed hemorrhoid and cut off its blood supply. This procedure is less painful than traditional hemorrhoidectomy and has a shorter recovery time. During the procedure, a circular stapling device is used to remove a ring of tissue from the rectum, which pulls the hemorrhoid back into place and reduces blood flow to the area. Patients typically experience less pain and faster recovery compared to traditional hemorrhoidectomy.
Laser Therapy:
Laser therapy uses laser energy to cut off the blood supply to the hemorrhoid, causing it to shrink and fall off. This relatively new treatment option is less common but can be effective for some patients. Laser therapy is minimally invasive and usually performed on an outpatient basis. The procedure involves using a laser to precisely target and coagulate the blood vessels feeding the hemorrhoid. Recovery is typically quick, with minimal pain and discomfort.

Home Remedies and Self-Care
In addition to medical treatments, various home remedies and self-care measures can help manage the symptoms of Grade 3 external hemorrhoids:
- Warm Sitz Baths: Sitting in warm water for 10-15 minutes several times a day can help reduce swelling and pain.
- Cold Compresses: Applying ice packs to the affected area can help reduce swelling and numb the area.
- Topical Treatments: Over-the-counter creams, ointments, and suppositories containing hydrocortisone or witch hazel can reduce inflammation and pain.
- Pain Relievers: Non-prescription pain relievers like acetaminophen or ibuprofen can help alleviate discomfort.
- High-Fiber Diet: Incorporating high-fiber foods into your diet can significantly reduce the occurrence of constipation and straining. Examples include fruits like apples and pears, vegetables like broccoli and carrots, legumes such as beans and lentils, and whole grains like oats and brown rice.
- Hydration: Adequate water intake is crucial. Aim for at least eight glasses of water a day to keep stools soft.
- Regular Exercise: Engaging in regular physical activity, such as walking, swimming, or yoga, can improve bowel function and reduce the risk of hemorrhoids.
- Avoid Prolonged Sitting: If your job requires long periods of sitting, take regular breaks to stand and move around. This helps alleviate pressure on the rectal veins.
- Healthy Bathroom Habits: Do not delay bowel movements when you feel the urge. Straining during bowel movements can be minimized by using a footstool to elevate your feet, which changes the position of your rectum for easier passage of stools.
Preventive Measures
Preventing external hemorrhoids involves addressing the underlying causes. Effective measures include:
- Maintaining a Healthy Diet: A diet high in fiber and low in processed foods can prevent constipation and reduce straining.
- Staying Hydrated: Drinking sufficient water helps keep stools soft and easy to pass.
- Regular Exercise: Physical activity promotes healthy bowel function.
- Avoiding Prolonged Sitting: Taking breaks and avoiding sitting for long periods can reduce pressure on the rectal veins.
- Proper Bathroom Habits: Avoiding straining during bowel movements and not delaying the urge to defecate can prevent hemorrhoid formation.
When to See a Doctor for External Hemorrhoid Grade 3: Comprehensive Overview.
It is essential to seek medical attention if:
- Symptoms Persist: If symptoms do not improve with home treatment or over-the-counter medications.
- Severe Pain: Intense pain or swelling requires medical evaluation.
- Excessive Bleeding: Persistent or heavy bleeding warrants a doctor’s visit.
- Changes in Bowel Habits: Significant changes in bowel habits or stool appearance should be investigated.
Psychological Impact
Living with Grade 3 external hemorrhoids can have a significant psychological impact. Chronic pain, discomfort, and the fear of bleeding can lead to anxiety and stress. It is important to address these psychological aspects as part of a comprehensive treatment plan. Counseling or therapy can be beneficial for managing stress and anxiety related to the condition.
Support and Resources
Support from healthcare professionals, including gastroenterologists and colorectal surgeons, is essential for managing Grade 3 external hemorrhoids. Additionally, support groups and online forums can provide valuable information and emotional support from others experiencing similar issues.
Conclusion:
Grade 3 external hemorrhoids, while more severe than earlier stages, can be effectively managed with a combination of lifestyle changes, dietary adjustments, home remedies, and medical treatments. Understanding the causes, symptoms, and treatment options allows for timely intervention and relief. By adopting preventive measures and seeking medical advice when necessary, individuals can manage and prevent the progression of hemorrhoids, leading to improved quality of life. Effective management also involves addressing the psychological impact of the condition and seeking support when needed.
While Grade 3 external hemorrhoids can be challenging to deal with, advancements in medical treatments and a comprehensive approach to care can provide significant relief and improve overall well-being. If you are experiencing symptoms of Grade 3 external hemorrhoids, it is important to consult with a healthcare provider to develop an individualized treatment plan tailored to your specific needs.